A strong response to antimicrobial resistance must include tackling TB.
Antimicrobial Resistance
Antimicrobial resistance (AMR)—which occurs when microorganisms no longer respond to the drugs designed to treat them—is becoming one of the defining health issues of our time. The threat posed by “superbugs” to public health, safety, and the global economy is staggering.
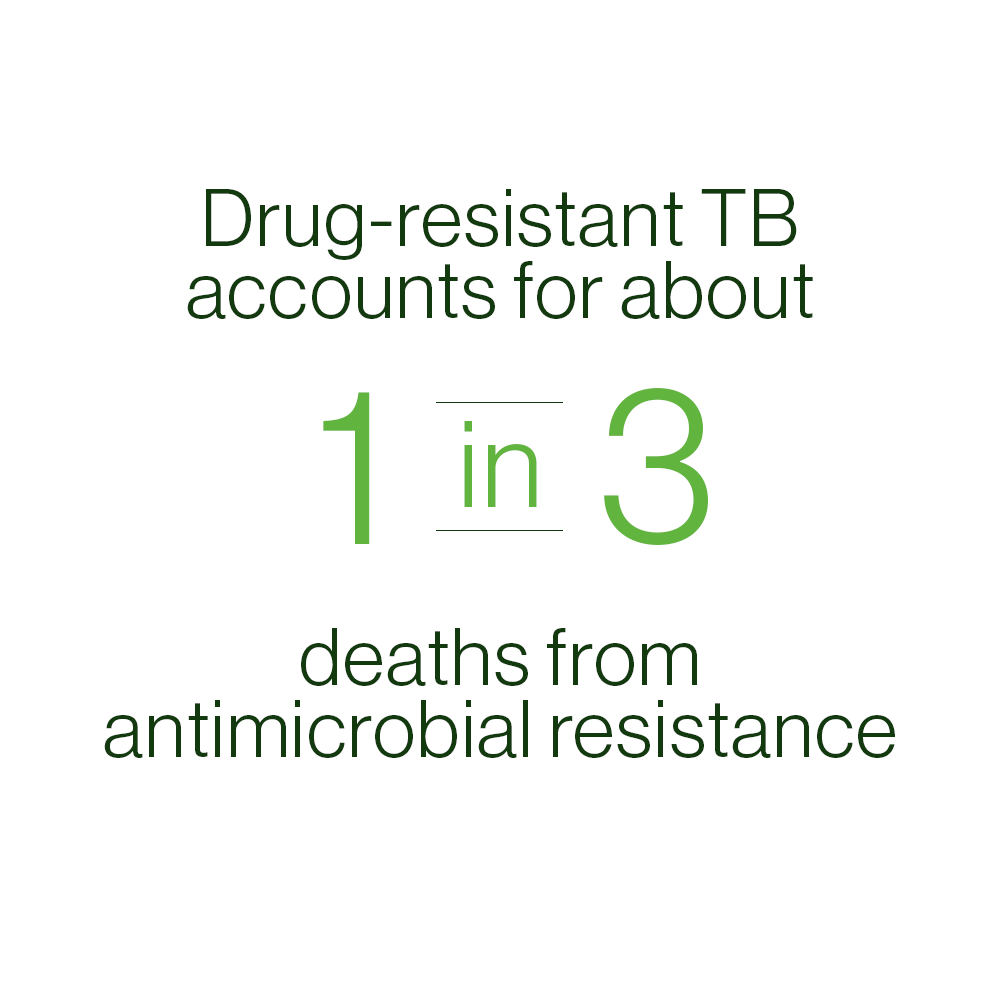
While AMR is often associated with hospital-based infections, like MRSA (methicillin-resistant Staphylococcus aureus), about 29% of deaths caused by antimicrobial infections today are due to drug-resistant TB. TB Alliance’s BPaL/M regimen for drug-resistant TB is a major win in the battle against AMR as well, leading to improved treatment success rates and reducing AMR-related deaths.
The World Health Organization’s (WHO) guidance on Country Preparedness for the Introduction and Appropriate Use of Antibiotics highlighted TB Alliance’s introduction as an example of an effective, rapid, responsible, and impactful introduction of a new drug (and regimen)
This is one day of traditional treatment for drug-resistant TB.
Today’s treatment can last two years or longer, is highly toxic, and ineffective.
The introduction of the BPaL/M regimens for DR-TB have already resulted in the saving of 11K lives and $100M. Over the next ten years, the regimen is projected to treat nearly 2 million people and save another $1.2B globally
A Growing Threat

MDR-TB:
MDR-TB, multidrug-resistant TB, is defined by resistance to the two most commonly used
drugs in the current four-drug (or first-line) regimen, isoniazid and rifampin. It is the result
of interrupted, erratic, or inadequate TB therapy, and its spread is undermining efforts to control
the global TB epidemic. Drug-resistant TB develops when the long, complex, decades-old TB drug
regimen is improperly administered, or when people with TB stop taking their medicines before the
disease has been fully eradicated from their body. Once a drug-resistant strain has developed, it
can be transmitted directly to others just like drug-susceptible TB. There were approximately 390,000
cases of drug-resistant TB in 2024.

XDR-TB:
Extensively drug-resistant tuberculosis, or XDR-TB, is a strain of tuberculosis, airborne and infectious, that is resistant to four commonly-used anti-TB drugs. Until the US FDA approval of pretomanid as part of the BPaL regimen, there was no reliable cure for XDR-TB. XDR-TB has been confirmed in 127 countries around the world and represents about five percent of all MDR-TB cases. XDR-TB is an extremely deadly and costly global health threat that the world must mobilize rapidly to tackle.
Dire Costs
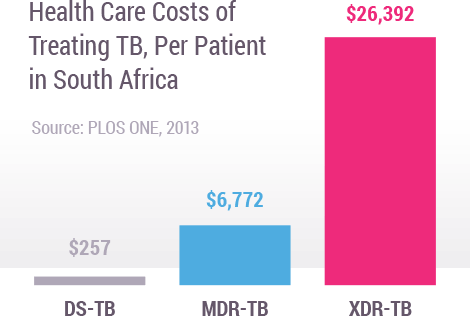
When infections become resistant to first-line drugs, more expensive therapies must be used to treat them. Lengthier treatment, often in hospitals, substantially increases health care costs as well as the economic burden on families and societies. The cost of treating a single case of MDR-TB or XDR-TB can be thousands of times more expensive than treating drug-sensitive TB. For example, in South Africa, drug-resistant TB consumed about 32% of South Africa’s US$218 million national TB budget (2011), despite the fact that it only accounted for about 2% of all TB cases.
Inadequate Treatment
BPaL/M is a six-month, all oral treatment for nearly all forms of DR-TB, but when treated with older regimens therapy for DR-TB is long, toxic, complicated and expensive.
6
Months
Months
Injections
1/day for at least 6 months.
9-24
Months
Months
Pills
12-24/day for as many as 24 months.
6-24
Months
Months
IV Infusions
2/day for 6-24 months.
14,000
Pills
Trillion Dollars
It takes 14,000 pills to treat one patient with drug-resistant TB.
Our Pipeline
To overcome treatment challenges, TB Alliance is developing the largest pipeline of new TB drugs in history.