Promising Trial Results Point to an Emerging Treatment Paradigm
Treatment for Every Person with TB
In 2016, TB Alliance realized significant progress in advancing new drug regimens that could significantly impact the TB pandemic. Results from the NC-005 trial and interim results from the Nix-TB trial point to the possibility of a new treatment paradigm where countries could use just two short, simple regimens to treat all people with TB, no matter their resistance profile.
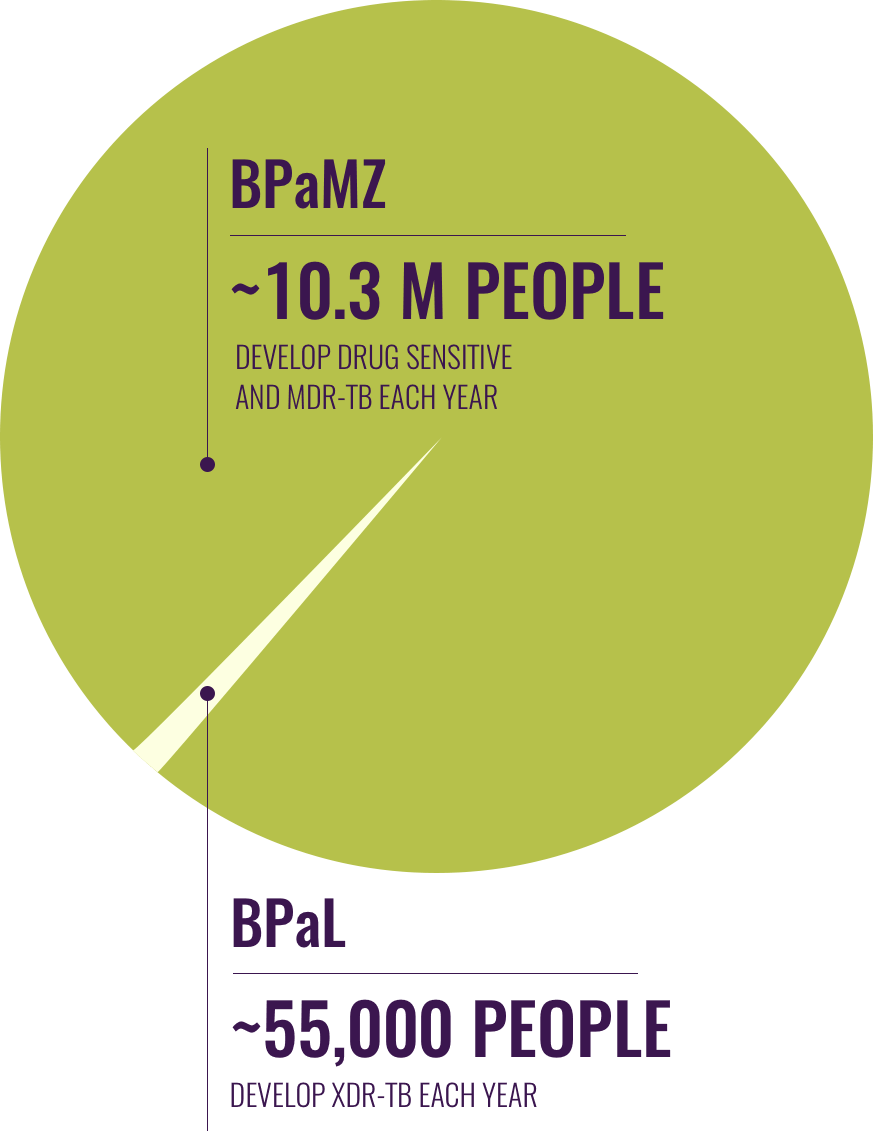
These regimens share two powerful new drugs--bedaquiline (B) and pretomanid (Pa), which TB Alliance began studying in combination in 2012. When B and Pa are paired with moxifloxacin (M) and pyrazinamide (Z) (BPaMZ), results show the regimen has promise to be a common therapy for virtually all patients with drug-sensitive TB and MDR-TB--which comprise the vast majority of TB patients. When bedaquiline and pretomanid are paired with linezolid (L) (BPaL), it creates a closely related treatment for the minority of patients who have the most deadly and difficult to treat TB, XDR-TB.
These two regimens have the potential to transform the treatment landscape. Both BPaMZ and BPaL can be maximally implemented with existing diagnostics, and countries might only need to stock a few oral drugs to treat all types of TB in treatment regimens of 4-6 months. That would be a major improvement from today, where countries devise regimens from more than 20 drugs and injections, which then must be taken for 6-24 months or longer, and, in drug-resistant TB, produce poor — if not dire — outcomes.
Results from the NC-005 and Nix-TB trials were presented at the 47th Union World Conference on Lung Health and at the 2017 Conference on Retroviruses and Opportunistic Infections (CROI).
Drug resistant TB is on the rise. New drugs are urgently needed.
NC-005 Trial: Promising results for
drug sensitive and MDR-TB
The BPaMZ regimen is poised to advance
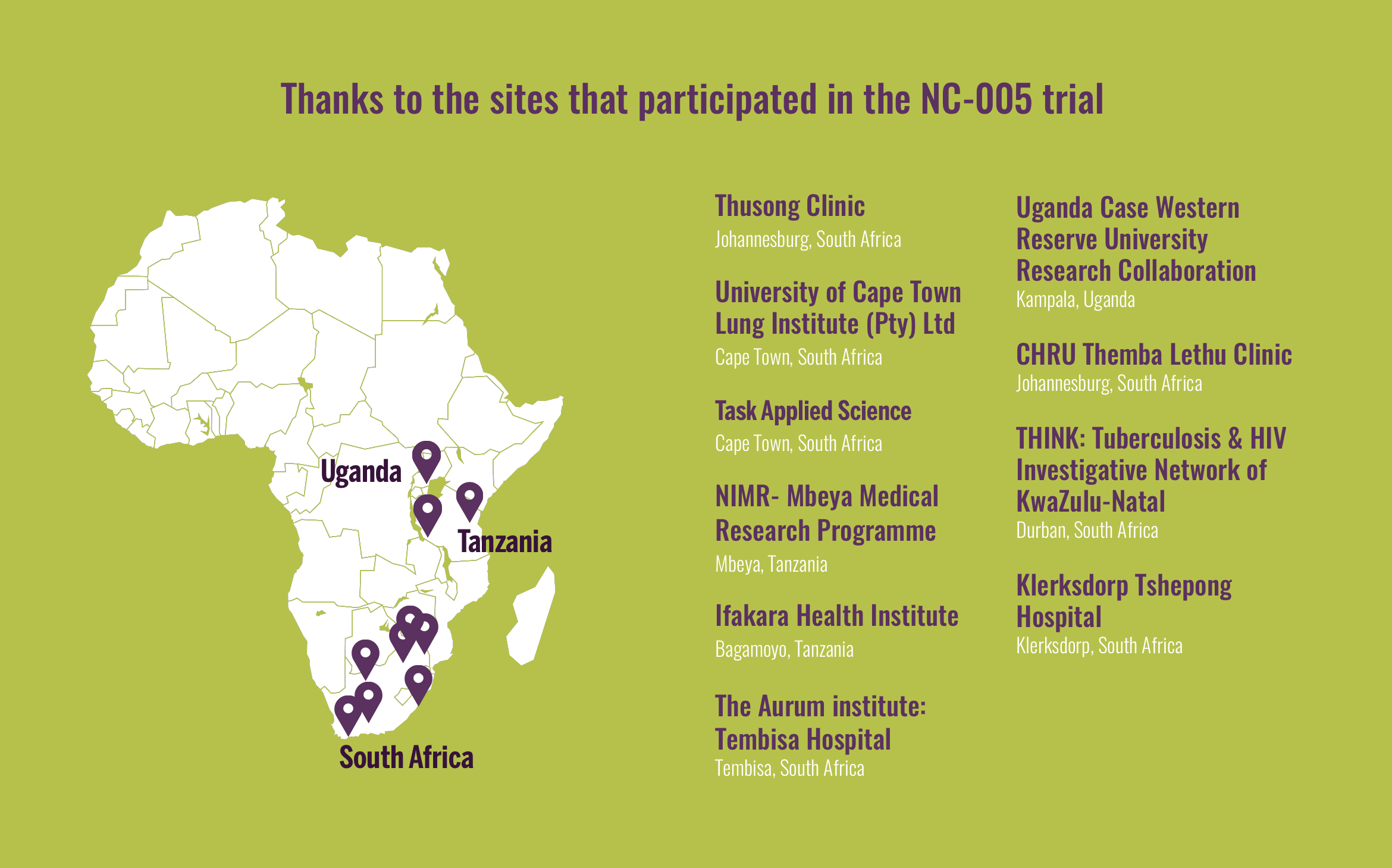
In 2016, TB Alliance reported the positive results of the NC-005 clinical trial. The trial examined drug combinations in patients with drug-sensitive TB and MDR-TB at 10 sites in Uganda, South Africa, and Tanzania. This Phase 2b study tested two different regimens of bedaquiline, pretomanid, and pyrazinamide (BPaZ), and in patients with MDR-TB, those three drugs with moxifloxacin (BPaMZ). The trial was initially launched in October 2014.
The patients in the trial who received a regimen consisting of all four drugs (BPaMZ) saw the quickest reduction in the amount of TB in their sputum. At the end of two months, MDR-TB trial participants cleared TB bacteria up to 3.5 times as quickly as the standard TB treatment regimen had done in drug-sensitive TB patients. In fact, more than three-fourths of patients taking BPaMZ were clear of TB bacteria after this initial two-month treatment (a range of 78-96% depending on whether their TB was fully sensitive to three or all four drugs in the regimen), compared with just 51% taking the standard first-line treatment.
The study also showed that it was possible to simplify the dosing of bedaquiline. Currently, bedaquiline is available in some countries with a dosing scheme of 400mg daily for two weeks, followed by 200mg three times a week for the remainder of a patient's treatment. This makes it difficult to combine bedaquiline into a fixed dose combination. The study found that a daily dose of bedaquiline (200 mg) is at least as active and safe as the labelled dose over a two-month time frame. This will allow for both simpler daily dosing with the regimen as well as incorporation into a fixed dose combination.
If successful in future trials, the BPaMZ regimen could offer a marked improvement over today's prevailing treatment regimens. The BPaMZ regimen could help rationalize and unify TB treatment by offering countries a single, 4-6 month, injection-free regimen that could treat the vast majority (estimated at approximately 99%) of patients. The regimen could be maximally implemented with diagnostics that are already available.
That would represent a major advance from today's current MDR-TB treatment which includes daily injections for six months and more than 14,000 pills over the course of 9 months to two years or even longer. Despite this arduous treatment, the survival rate of those who are able to access the current MDR-TB treatment is only about 50%.
Today, more than one in four deaths caused by antimicrobial resistance are attributed to drug-resistant tuberculosis. The utility and urgency of one simple regimen to treat the majority of patients is already apparent. As the problem of drug resistance continues to grow, improved regimens are an imperative, not only in terms of the financial costs and burden on the healthcare sector, but also the moral imperative to save lives.
Additional research is now being planned and funding is being sought to further advance the BPaMZ regimen.
Redirecting Resources for Impact
The promising results of the NC-005 trial and the BPaMZ regimen have compelled TB Alliance to revise its clinical trial plans and redirect its resources to advancing a regimen that has the most potential for impact. As a result, TB Alliance announced in December 2016 that the STAND trial, which is testing the PaMZ regimen, would not re-open enrollment to new patients.
While both the BPaMZ and PaMZ regimens show potential to improve treatment, results show that BPaMZ could improve treatment for significantly more patients, including those with drug-sensitive TB and virtually all patients with MDR-TB, and appears to have greater potential than PaMZ to shorten treatment. Of the 284 patients enrolled in the STAND trial, all have now completed treatment and the initial six-month follow up period. TB Alliance will continue to follow all the patients in the trial for two years as per the original study design. All the associated data will be collected and analyzed, and we will report findings from the trial.
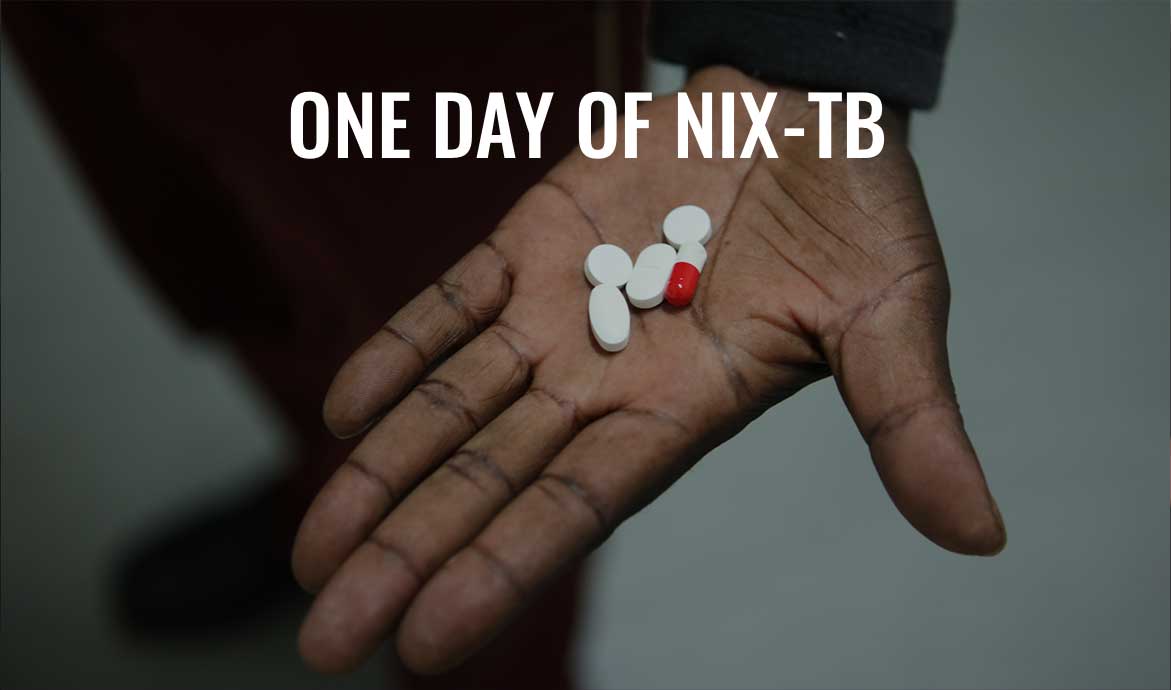
The Nix-TB trial: Promising
Treatment for XDR-TB
Stakeholders Speak about Nix-TB
The first couple of patients, we wondered— Dr. Pauline Howell, Sizwe Tropical Diseases Hospitalis it going to hold? Are they going to stay culture negative?...and then we just realized, this is what these drugs do. They cure people.
Testing the BPaL regimen
Today, less than 1 in 3 people survive with XDR-TB therapy — and those dismal statistics reflect only those who are able to access treatment. XDR-TB therapy can consist of six months of daily injections alongside two years or more of a daily drug cocktail consisting of a dozen pills or more. These regimens — really, last-ditch salvage treatments — are often accompanied by debilitating side-effects like deafness and psychosis. However, interim results from the Nix-TB (New Investigational Drugs for XDR-TB) trial show the exciting potential to markedly transform treatment of XDR-TB into a readily treatable and curable disease.
Nix-TB tests a three-drug regimen consisting of bedaquiline, pretomanid, and linezolid (known together as BPaL). Early data from the Nix-TB trial indicate the potential to treat XDR-TB in just six months with a dramatically simpler, safer, and more effective regimen. By the end of 2016, the trial had admitted 65 participants into two trial sites in South Africa, Sizwe Hospital in Johannesburg and Brooklyn Chest Hospital in Cape Town. To date, 34 patients have successfully completed the six-month course of treatment and six months of follow up. Patients will continue to be closely monitored for two years after completing their BPaL regimen. The Nix-TB trial was launched in May 2015. An additional study on early bactericidal activity of linezolid helped to improve understanding of the drug and will inform future testing of the BPaL regimen.
Building on the promising interim results of the BPaL regimen in Nix-TB, TB Alliance is working to advance this treatment as quickly as possible. We expect to launch the ZeNix trial in late 2017. This clinical trial will seek to optimize the use of linezolid in the regimen, including determining the best dose and treatment duration needed to ensure safe, effective treatment while minimizing side-effects. The ZeNix trial is expected to be conducted across 10 trial sites in South Africa, Georgia, Belarus, and Russia. Patients will continue to be enrolled in the Nix-TB trial until the ZeNix trial can be opened.
At the same time, TB Alliance is now planning for the development of a patient access program for the BPaL regimen, working with partners to develop a framework in which patients with urgent medical needs are able to access this ground-breaking treatment prior to regulatory approval. If funding can be secured, TB Alliance will be the first product development partnership to offer such a program.